2nd International Conference on Obesity and Weight Loss
October 15-17, 2018, Amsterdam, Netherlands
Hypothalamic Obesity & Craniopharyngioma
Hamad General Hospital and Qatar Metabolic Institute, Qatar
Obesity is a common complication after craniopharyngioma therapy, (75% of survivors), The hypothalamus is the anatomic seat of peripheral energy regulation.When the hypothalamus is damaged, a syndrome of intractable weight gain might occur “hypothalamic obesity,”
Hypothalamic obesity syndrome has also been reported in Pseudo tumor cerebri, Head Trauma and Infiltrative or inflammatory diseases of the hypothalamus.
Hypothalamic obesity due to craniopharyngioma can occur in response to any hypothalamic damage.
It can occur due to : Craniopharyngioma tumor itself, Surgery to extirpate it, subsequent radiation therapy. Extremely high frequency of hypothalamic obesity (30– 77%) has been documented after craniopharyngioma treatment. Pathogenesis of Hypothalamic obesity Syndrome is related to the Inability to transduce afferent hormonal signals of adiposity, in effect mimicking a state of CNS starvation.
Efferent sympathetic activity drops, resulting in malaise and reduced energy expenditure
Increased vagal activity, resulting in increased insulin secretion and adipogenesis.
children with hypothalamic obesity exhibit weight gain, even in response to forced caloric restriction.
This seems paradoxical, as one would expect that if hyperphagia were the reason for the obesity, then caloric restriction would be effective in preventing further weight gain.
Best treatment is prevention, as Hypothalamus is extremely sensitive to both surgical intervention and/or external beam radiation.
Rather than employing gross total or subtotal resection as a primary therapy for some posterior fossa tumors, newer strategies have been developed which treat them more conservatively, using stereotactic biopsy and conformal irradiation.
The use of serotonin or norepinephrine reuptake inhibitors (e.g., fluoxetine) have only salutary efficacy. These medications work centrally to reduce food intake, but not energy expenditure, thus have limited value.
Dextro amphetamine 5mg PO bid, acts both centrally and peripherally, achieved weight stability.
Leptin therapy has been ineffective for weight loss but rather may show some success in weight maintenance
To enhance insulin action, somatostatinanalog “octreotide” was examined. Octreotide15 µg/kg/day subcutaneously resulted in insulin suppression and stabilization of BMI, decreased leptin, decreased caloric intake, increased spontaneous physical activity, and improvement in quality of life.
Recently, bariatric surgery (RYGB, LSG, and truncal vagotomy) have also been attempted with various success outcomes.
Biography:
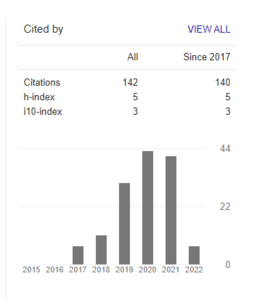
Dr. Mohamed Aly Elsherif earned his master and doctorate degrees in internal medicine and diabetes at Tanta University, Egypt and continued his interest in endocrinology by earning master of endocrinology from the University of South Wales, UK. He completed his fellowship training in internal medicine at Tanta Medical School. He worked as specialist internist in health insurance hospital and consulted on endocrinology and diabetes in MDH hospital in Saudi Arabia. He chaired internal medicine department in 2 private hospitals is Saudi Arabia for 4 years and moved to Qatar to continue his interest in clinical management of metabolic and endocrinal disorders with special focus on diabetes and obesity management. Dr Elsherif has a clinical experience of more than twenty years in the field of endocrinology, diabetes and obesity management. He is internationally recognized by World Obesity Federation as a certified obesity health professional holding SCOPE certificate. Dr. Elsherif is now an associate consultant in bariatric endocrinology, working in bariatric and metabolic surgery department Hamad General Hospital and Qatar metabolic institute. He has a great interest in teaching as well as research activities and has several research studies published in high impact journals and presented in international conferences. Dr. Elsherif practiced his interest and experience in teaching and was selected by HMC medical education to be one of the instructors of communication skills and other educational courses, he was also invited as a speaker in local and international conferences