Research Article
Assessment of Antenatal Care services among Pregnant Women in Omani Polyclinics
School of Pharmacy, College of Pharmacy and Nursing, University of Nizwa, Oman
*Corresponding author: Hameed Swadi Hassan, Associate Professor, School of Pharmacy, College of Pharmacy and Nursing, University of Nizwa, Birkat Al-Mouz, Nizwa, Oman, E-mail: hameed@unizwa.edu.om
Received: April 2, 2019 Accepted: April 25, 2019 Published: May 3, 2019
Citation: Al-Abri HA, Al-Balushi IM, AL-Malki SR, et al. Assessment of Antenatal Care services among Pregnant Women in Omani Polyclinics. Madridge J Nurs. 2019; 4(1): 145-150. doi: 10.18689/mjn-1000126
Copyright: © 2019 The Author(s). This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background: Since the antenatal care is important screening for the health of the pregnant woman and the child to achieve the best possible outcome, it is chosen to assess this screening in 6 government polyclinics in different regions in Oman during January 2011.
Method: This retrospective study was carried out in six different regions in Oman by using the available data of 6 polyclinics. The results are reported according to a prepared data collection forms for 1200 Omani pregnant women during January 2011. Data collection forms were designed and included demographic parameters and other parameters chosen from similar previous studies. All the obtained results are presented in tables region wise.
Results: The age of the investigated pregnant women in this study was found to range from 18-49 years with a majority (65.8%) of 20-35 years and about 80% of them were from urban areas. The weight of the pregnant women varied from 60-80 kg in the majority of cases (63%). 36% of the pregnant women were primigravida and the remaining 64% were multigravida in the different chosen regions. About 60% were found educated with various school levels and around 70% were unemployed. The majority of the pregnant women showed normal blood pressure measurements and audible fetal heart sounds from the 3rd month of pregnancy onwards.
The laboratory investigations that were carried out for the pregnant women included the blood sugar monitoring, haemoglobin and showed normal values in the majority of cases. Urine test was found normal in about 85% of the pregnant women and only few cases (15%) showed signs of urinary tract infection (UTI).
Complications of pregnancy that recorded in some investigated women were found varied and differ from one region to another. The commonest associated complication was headache. Other minor complications included itching, dysuria and gestational diabetes. Few cases, however, were found to suffer from difficulty in breathing and leg oedema.
Besides the nutritional supplements which were found to be prescribed for all investigated pregnant women, some other medications were reported to be used by different women. These include analgesics (paracetamol) in majority of cases, followed by antihistaminic, urine alkalizers and antibiotics. The overall impression is that the antenatal care (ANC) services provided to the pregnant women during the period of study were adequate and satisfactory.
Keywords: Pregnant women; Antenatal care; Complications; Medications; Oman.
Introduction
Antenatal care is the clinical assessment of the pregnant women and her fetus to attain the best possible outcome [1]. Normal pregnancy is usually considered as a state of health and frequently accompanied by some symptoms which may at other circumstances regarded as signs of illness. Nausea, vomiting, heart burn, constipation and leg cramps are not life threatening or hazardous to mother or baby [2].
Pregnancy may be suspected by the women based on her knowledge of her menstrual cycle and the signs and symptoms of pregnancy. Women may confirm their pregnancy using a home pregnancy test or may also be sought from the midwife or the doctor. This is established by a detailed history and relevant clinical examination based on signs and symptoms of pregnancy [3].
Historically, antenatal care has begun in Paris in 1788 at two shelter homes for abandoned women. Later, and during the 1st decade of this century it is thought to have originated in Boston, USA. Before that time, pregnant women may have visited a clinic to confirm her pregnancy but did not attend the clinic again until the time of delivery. In 1919, antenatal care services started in England by midwifery service and home visiting nurse. These services became so popular in England and Walesʼs so that about 77% of the total registered birth have been provided with these services and about 69.8% of pregnant women received an early home visit by a health visitor. Afterwards, the World Health Organization (WHO) expert committee on maternal and child health defined maternity care which was approved with minor amendments and continued as a universally accepted standard today [4].
The aims of the antenatal care have been pointed out by so many authors. Among these antenatal care promotes and protects the health of pregnant women, detects high risk cases and gives them special attention, foresees complications and prevents them, eliminates anxiety associated with pregnancy, reduces maternal and infant mortality and morbidity and advises the pregnant women about elements of child care, nutrition, hygiene and sanitation [5,6].
Steps to healthy pregnancy, in general, include early prenatal care, good diet including vitamins, regular exercise, quitting smoking, avoiding alcohol and drugs, elimination of environmental stress and good general hygiene [7,8].
All pregnancies carry certain risks to both mother and baby [2]. Some of these risks may present before pregnancy and others may develop during the pregnancy. Both can be regarded as high risk problems. The maternal risk factors include women age; young or old, overweight or underweight, previous abortion, stillbirth or preterm labour. They may also include preexisting health conditions such as high blood pressure, diabetes or AIDS. Women who were extremely healthy before pregnancy may also develop these problems during the period of the pregnancy [2]. Fetal factors may include exposure to infection, medications, addictive substances and serious health problems like a heart defect [7,9].
The suggested optimum number of visits of pregnant women to antenatal clinics may be classified as monthly visit since the diagnosis of pregnancy until 28 week of pregnancy, bi-monthly visit until 36 week of pregnancy and then weekly visit during the last four weeks of pregnancy. More visits may be necessary if an existing medical problem or associated complications are encountered [8].
The pregnant woman usually has a medical examination carried out by obstetrician once her pregnancy is confirmed. This medical examination includes general appearance of the pregnant woman, general examination of the mouth and mucous membranes, height, weight, blood pressure, blood tests that include full blood count, blood group, blood glucose, haemoglobin, hepatitis B and HIV screening. The urine analysis also generally carried out as a routine investigation. Breast examination, the heart and the lungs, and examination of legs for varicose veins and oedema are also performed as part of the medical checkup [4]. Fetal status also should be checked, to ensure that the status of the fetus inside the uterus is normal, during the medical examination [10].
Oman is an Arabic country with a total population of 4,947,052 out of which only 2,947,052 is Omani. The remaining 2,000,000 is expatriates [11]. Child health programs in Oman are considered to be successful. Before 1970, infant mortality in Oman was estimated to be around 214 out of 1000 births, which later by 1992 reduced to 25 [12]. The world Health Organization (WHO) has recognized Oman and ranked it 8th best for its health care system [12]. Also, the United Nations Childrenʼs Fund recognized Oman as the most improved country among 135 countries during 1970-2010 [13]. Such substantial improvements may be attributed to the rapid socioeconomic development of Oman and to the health plan of the Ministry of Health. The Ministry of Health has introduced maternal and child health services into the field of the primary health care during 1987 [14] and since 2001, the Ministry of Health has implemented many strategies to reduce morbidity and mortality [15]. According to the Oman Annual health report for 2012, the average number of antenatal care visits for registered pregnant women was 6 [14]. The antenatal care coverage for at least one visit has increased to 99.4%, whereas for 4 or more visits it reached 80.4% in 2012, and booking during the 1st trimester reached 66.5% [14]. However, regional variations in the proportions of antenatal care coverage and those registered in the 1st trimester have been observed.
Need for the study
Since the antenatal care is important screening for the health of the pregnant woman and the child to achieve the best possible outcome, it is chosen to assess this screening in 6 government polyclinics in different regions in Oman during January 2011.Therefore, the objective of this study is to assess the quality of the antenatal care services and the socio-demographic characteristics of pregnant women in the polyclinics in order to help policy makers in the Ministry of Health to adapt their policies and strategies regarding maternal health services.
Materials and Methods
The present study is to assess the antenatal care services among the pregnant women attending government polyclinics with the use of data collection forms. This study was accepted by the graduation project committee of the School of Pharmacy, College of Pharmacy and Nursing, University of Nizwa (as a graduation project study) and approved by the Dean of the College.
Six polyclinics were chosen in different Willyates in Oman. These regions include Nizwa, Bahla (AL-Dakhylia), Sohar, ALSuwaiq (North Al-Batina), Barka (South AL-Batina), and Bidaya (AL-Sharqiya). The study was conducted during January 2011 as a retrospective study using the dataset of the government polyclinics. The prepared data collection forms for such purposes included demographic parameters; the participantʼs age, weight, parity and the records of the blood pressure, fetal hart sounds, and blood groups in addition to other variables concern with the findings of laboratory investigations of blood sugar, haemoglobin, and urine analysis. Medical problems associated with the pregnancy and medications used during pregnancy were also reported in this study.
A total of 1200 pregnant women (200 in each polyclinic) were chosen in this study. The used data collection forms, in this study, were based on similar previously conducted studies [16] with some modifications. All the obtained results are tabulated region-wise.
Results
The age of the investigated pregnant women in this study was found to range from 18-49 years with a majority (65.8%) of 20-35 years and about 80% of them were from urban areas. The weight of the pregnant women varied from 60-80 kg in the majority of cases (63%). 36% of the pregnant women were primigravida and the remaining 64% were multigravida in the different chosen regions. About 60% were found educated with various school levels and around 70% were unemployed.
The majority (88%) of the pregnant women showed normal blood pressure measurements of 120/75 mmHg. Fetal heart sounds were positive in 97% of cases from the 3rd month onwards and ranged from 110-160 bpm.
The laboratory investigations that were carried out for the pregnant women included the blood sugar monitoring, haemoglobin, and urine analysis and showed that 79% were with normal blood sugar level (4.0-9.2 mg/dL), and the remaining 21% were with high blood sugar level. The haemoglobin value was seen to range from 9-14 gm/dL with an average of 11-14 gm/dL in the majority (72%) of the pregnant women investigated. However, the remaining women (28%) showed less hemoglolobin value; less than 11 gm/dL. Urine test was found normal in about 85% of the pregnant women encountered in this study and only few cases (15%) showed signs of urinary tract infection (UTI).
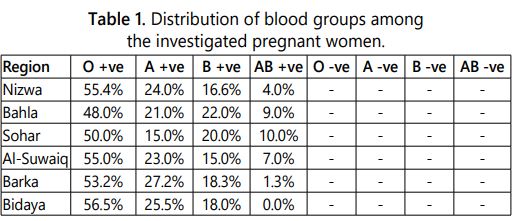
The distribution of blood groups in the investigated pregnant women showed a dominance of O-positive blood group in about more than 50% of cases. The AB-positive blood group showed the very least percentage. No negative blood groups were detected however (Table 1).
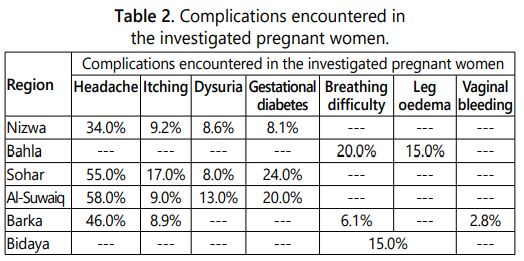
The complications encountered during the period of the pregnancy and recorded in some investigated women, in the different regions, were also found varied and differ from one region to another. The commonest associated complication was headache. The remaining complications included itching, dysuria and gestational diabetes. Few cases, however, were found to suffer from difficulty in breathing and leg oedema as shown in table 2.
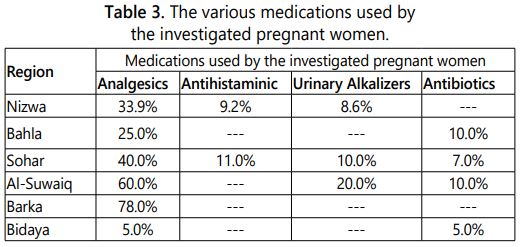
Besides the nutritional supplements (vitamins, ferrous sulphate and folic acid) which were found to be prescribed for all investigated pregnant women, some other medications were reported to be used by different women. These include analgesics (paracetamol) in majority of cases, followed by antihistaminic, urine alkalizers and antibiotics as shown in table 3.
Discussion
Adequate utilization of antenatal care services by skilled health care providers can help to ensure reduction in maternal and child morbidity and mortality. Several studies have shown that motherʼs socio-demographic factors affect the adequacy of antenatal care utilization [17-19]. A systematic review in developing countries showed that adequate antenatal care utilization cannot be achieved only by establishing health centres alone but, womenʼs overall social, political and economic status should be considered [20]. For better evaluation of the adequacy of antenatal care, valid indicators are needed. Unfortunately, there is no consensus on the parameters used for evaluation of the adequacy of antennal care. Most studies include the number of antenatal care visits and timing of first visit during the 1st trimester [17,19,21]. In addition to these, core services performed at least once during pregnancy and the provider of antenatal care as well as the place of delivery has to be included into the process of evaluation [19,16].
The age of the investigated pregnant women in this study was found to range from 18-49 years with a majority (65.8%) of 20-35 years and about 80% of them were from urban areas. In comparison to a recent study, in Oman [22], the majority (56.8%) of women investigated was in the age group of 25-34 years and most of them (71.5%) were from urban areas. In Australia [23], the mean age of the pregnant women presented as 27 years and in Nigeria, a record of mean age of 25 years of pregnant women was also presented [24]. The effect of motherʼs age on adequacy of number of antenatal care visits is inconsistent across the literature, however [22].
A study from Bangladesh [25] revealed that more young pregnant women (less than 20 years) had the higher use of the antenatal care service than those of 35-49 years. In South India [26], the reverse is true where young mothers (25-29 years) were less likely to utilize antenatal care service than old women. In other studies, in certain parts of India and Egypt, the mother age was not seen as a determining factor for adequate number of antenatal care visits [27,28].
In Japan, it was reported that only 83% of cases have attended the antenatal care clinics [29]. The mean gestational age of attended women at 1st visit was about 4 months and were found to have lower incidence of preterm delivery, pregnancy induced hypertension, emergency caesarian section and low birth weight.
In Kassala, eastern Sudan, the antenatal care coverage showed that 90% of women had at least one visit [30] and about 59.6% of them attended in the 1st trimester, 37.4% in the 2nd trimester and only 3.1% in the 3rd trimester.
A significant association was found between women pregnant with the 1st baby and having adequate number of antenatal care visit or early use of antenatal care [22]. Such association also reported from Egypt, Syria, Kenya and India [17,28,31,32]. Other factors such as motherʼs education, socioeconomic status, residence and employment have not been seen to be associated with adequacy of antenatal care visit and early use of antenatal care [22]. In other studies, a positive association was found between these factors and adequate number of antenatal care visit and early antenatal care use [17,28,31,32]. The discrepancy between these studies could be attributed to, as reported, the intention of the Omani authorities to implement the Health for all strategy through the primary health care in its 6th five-year plan [22]. In our study, the association between the 1st pregnancy and adequate number of antenatal care or its early use, although reported by some studies, has not been investigated, however. Again some useful data like health education provided, vaccination of the mothers, sex and language of the antenatal care provider which were regarded as limitations in some studies [22] have not been highlighted or covered, in our study, however.
There is an increasing use of antenatal care in Bangladesh [33,34]. The proportion of women receiving antenatal care increased from 28% in 1993 to 60% in 2007. Educated women were more likely receiving antenatal care than uneducated women. A low coverage of antenatal care was also reported in Darfur, Sudan, where 41.8% of the surveyed women had not attended antenatal care at all [30]. In Pakistan, also, only 30% of women were found to utilize the antenatal care service [35].
In Australia and elsewhere, an evidence approach to develop guidelines to improve the quality of antenatal care has been increasingly promoted [36,37]. Recommendations about syphilis testing were found consistent with local protocols, national polices and research evidence. But for other diseases, like gestational diabetes mellitus (GDM) and HIV testing, there were inconsistent policies [38,39]. Smoking cessation information and advice were also rarely included despite its effectiveness in improving the outcomes. Also, national policies about the number of routine visits have not been identified.
Women with a low haemoglobin level during the 1st and 2nd trimester have been shown to be exposed to high risk of preterm birth [40]. Among women with normal range of haemoglobin level, the unadjusted rate of preterm birth was 8% during the 1st trimester. This rate has been found to represent 11-15% among women with low haemoglobin level. Similar rate of preterm birth was reported during the 2nd trimester in regards to normal and low haemoglobin levels. Low maternal haemoglobin level during the 3rd trimester was not associated with increased risk of preterm birth. In our investigated sample, most (72%) of the women were found with normal haemoglobin value and no preterm birth assessment was investigated, however. In regards to the variables of the antenatal care, all surveyed women, in this study, were found to be investigated for haemoglobin, blood sugar, blood pressure measurement, blood groups distribution, and urine analysis. Ultrasonography, although it is essential in some cases, was not included in our survey, however.
A study conducted in Indonesia in 2002-2003 and 2007 revealed that most of the sample (91%) did not develop any complications during pregnancy. Their weight, blood pressure and urine analysis were checked on 97.3%, 95.1% and 86.3% respectively [41]. In Canada (1993-2003), the most common medical problems that pregnant women encountered were threatened preterm labour, antenatal haemorrhage, hypertension, vomiting and diabetes [42]. Counselling about dangers of pregnancy was reported by approximately 3/4 of the pregnant women in the recent study [22]. This was higher than what was reported in other studies such as Tanzania, where less than 1/2 of the pregnancy danger signs were recalled by clients [43]. In our investigated sample, however, headache, itching, dysuria, gestational diabetes, breathing difficulties leg oedema and minor vaginal bleeding were reported among the women in different regions.
Lack of awareness of the complications of pregnancy was also noted. National statistics in Oman showed an increasing rate of low birth weight from 4.1% in 1980 to 9.5% in 2012 [14]. The abortion ratio per 1000 live births showed a slow decrease from 150 in 1995 to 134 in 2012. The proportion of caesarian sections increased from 5.1% in 1990 to 17.5 % during the same period. Although anaemia among pregnant women decreased from 42.8% in 2000 [44] to 26.7 in 2012, the rate is still high [14]. In addition other forms of morbidity associated with pregnancy like diabetes mellitus and hypertension have increased to 4.8% and 1.1% respectively. Government health care personnel in India [45] provide iron and folate supplements for pregnant women. High proportion of pregnant women (85%) in India receiving iron supplements regularly. In other studies, iron pills thought to cause the child to be dark-skinned and this widespread belief often urges the pregnant women to discontinue. However, in our investigated sample, it was found that all cases relied on nutritional supplements, including iron.
The association between parity and adequacy of antenatal care was reported to be negative in some studies [18,46]. In others, however, no relation was found at all [47]. Inadequate antenatal care among high parity women could be due to time management problems, negative attitudes resulting from previous pregnancies or knowledge and experience gained from previous pregnancies [22]. In our sample, however, the multigravida women represented by 36% compared to 21.61% [22] and all appeared to utilize antenatal care services more than the primigravida.
The distribution of the blood groups in this study did not differ from what was reported earlier where there is a dominance of O+ blood group among the Omani population [48].
In spite of the good health status of women in Oman, there is still need for further improvement according to the National Health Survey in 2000 [45] and the Reproductive Health Survey in 2008 [49].
All investigated women in the present study appeared to receive antenatal care by skilled health care providers (doctors) in the chosen government polyclinics. There is ample evidence that antenatal care represents an opportunity to deliver interventions that will improve maternal health, perinatal health and more than likely, perinatal survival.
Conclusion
Based on the obtained results, it was found that the antenatal care services in the 6 different chosen polyclinics were adequate and satisfactory. All the records showed full screening of the attended pregnant women. Most of the attended women ranged from 20-35 years and the majority were from urban areas. Also, the majority were multigravida in the different chosen regions.
The required laboratory investigations that are carried out to the pregnant women showed normal values in the majority of cases. The expected complications of pregnancy that recorded in some investigated women varied and differ from one region to another. In addition to the nutritional supplements which were found to be prescribed for all investigated pregnant women, some other medications were reported to be used according to the complication (s) encountered.
Recommendations
Based on this study, as well as other studies, we would like to recommend, in general, that inter conception care should be used to provide additional intensive interventions to women who have had previous pregnancy with an adverse outcome (i.e. infant death, fetal loss, birth defects, low birth weight or preterm birth). Also, risk assessment and educational and health promotion counseling should be applied to all women of childbearing age to improve pregnancy outcome. Lastly, public awareness of the importance of preconception care services should be addressed by using information and appropriate tools, health literacy and cultural contexts.
Acknowledgment
We are indebted to the college of Pharmacy and Nursing, University of Nizwa for offering this opportunity to conduct this research via the provision of the academic programs. Our thanks are also extended to the respected directors of the polyclinics for their valuable help in providing the access to the available data sets in the chosen polyclinics.
References
- Prenatal care. Accessed on March 28, 2019.
- Weber JR. Nurseʼs handbook of Health Assessment. Wolters Kluwer Health/Lippincott Williams and Wilkins; 2007.
- Elizabeth M. Midwifery for Nurses. CBS Publishers & Distributors; 2009.
- Effendi R, Isaranurug S, Chompikul J. Factors related to Regular Utilization of Antenatal Care Service Among postpartum Mothers in PasarRebo General Hospital Jakarta, Indonesia. Journal of Public Health and Development. 2008; 6(1): 113-122.
- Facello DC. Maternal/fetal attachment: associations among family relationships, maternal health practices, and antenatal attachment. West Virginia University; 2008.
- Almstrom H, Granström L, Ekman G. Serial antenatal monitoring compared with labor induction in post-term pregnancies. Acta Obstet Gynecol Scand. 1995; 74(8): 599-603.
- Jolly M, Sebire N, Harris J, Robinson S, Regan L. The risks associated with pregnancy in women aged 35 years or older. Hum Reprod. 2000; 15(11): 2433-2437.
- Nizalova OY, Vyshnya M. Evaluation of the impact of the mother and infant health project in Ukraine. Health Econ. 2010; 19: 107-125. doi: 10.1002/hec.1609
- Meyers SE. Maternal Role & High-Risk Pregnancy Experience with Antepartum Hospitalization. The University of Texas School of Nursing at Houston.
- Agarwal P, Singh MM, Garg S. Maternal health-care utilization among women in an urban slum in Delhi. Indian J Community Med. 2007; 32(3): 203-205. doi: 10.4103/0970-0218.36829
- Wikipedia.org. Demographics of Oman. 2019.
- Al-Sinani M. Breast feeding in Oman-The way forward. Oman Med J. 2008; 23(4): 236-240.
- United Nations Childrenʼs Fund. Oman: Country programme document 2012-2015. Geneva; 2011.
- Abd El Hamid M, Al Husseni H, Moussa M. Effects of sociodemographic factors on maternal health care services in some Arabian countries. A comparative study based on the results of the Pan Arab Project for Family Health. In: Proceedings of the First Arab Conference on Family Health and Population. 2006; 2: 227-265.
- Bashour H, Abdulsalam A, Al-Faisal W, Cheikha S. Patterns and determinants of maternity care in Damascus. East Mediterr Health J. 2008; 14(3): 595-604.
- Ribeiro ER, Guimarães AM, Bettiol H, et al. Risk factors for inadequate prenatal care use in the metropolitan area of Aracaju, Northeast Brazil. BMC Pregnancy Childbirth. 2009; 9: 31. doi: 10.1186/1471-2393-9-31
- Tran TK, Gottvall K, Nguyen HD, Ascher H, Petzold M. Factors associated with antenatal care adequacy in rural and urban contexts-results from two health and demographic surveillance sites in Vietnam. BMC Health Serv Res. 2012; 12: 40. doi: 10.1186/1472-6963-12-40
- Simkhada B, Teijlingen ER, Porter M, Simkhada P. Factors affecting the utilization of antenatal care in developing countries: systematic review of the literature. J Adv Nurs. 2008; 61(3): 244-260. doi: 10.1111/j.1365-2648.2007.04532.x
- United Nations Population Fund. Potential contributions to the MDG agenda from the perspective of ICPD. A reference guide to evidence for policy dialogue in the LAC Region; 2007.
- El Aty A, Meky FA, Morsy M, El Sayed MK. Overall adequacy of antenatal care in Oman: secondary analysis of national reproductive health survey data, 2008. East Mediterr Health J. 2015; 20(12): 781-788.
- Rumbold AR, Cunningham J. A review of the impact of antenatal care for Australian Indigenous women and attempts to strengthen these services. Matern Child Health J. 2008; 12(1): 83-100. doi: 10.1007/s10995-007-0216-1
- Osungbade KO, Shaahu VN, Uchendu OC. Clinical audit of antenatal service provision in Nigeria. Health Care Women Int. 2011; 32(5): 441-452. doi: 10.1080/07399332.2010.517878
- Temple P, Lutenbacher M, Vitale J. Limited access to care and home healthcare. Clin Obstet Gynecol. 2008; 51(2): 371-384. doi: 10.1097/GRF.0b013e31816f2952
- Bloom SS, Lippeveld T, Wypij D. Does antenatal care make a difference to safe delivery? A study in urban Uttar Pradesh, India. Health Policy Plan. 1999; 14(1): 38-48.
- Gupta A, Chhabra P, Kannan AT, Sharma G. Determinants of utilization pattern of antenatal and delivery services in an urbanized village of East Delhi. Indian J Prev Soc Med. 2010; 41(3&4): 240-245.
- Farahat T, Esam M, Alkot M, Shaheen H, Abd-Elgwad F. Determinants of antenatal care utilization in Menofia Governorate, Egypt. Egypt J Community Med. 2012; 30(1): 1–10.
- Alexander GR, Kotelchuck M. Assessing the role and effectiveness of prenatal care: history, challenges, and directions for future research. Public Health Rep. 2001; 116(4): 306-316. doi: 10.1016/S0033-3549(04)50052-3
- Ali AA, Osman MM, Abbaker AO, Adam I. Use of antenatal care services in Kassala Eastern Sudan. BMC Pregnancy Childbirth. 2010; 10: 67. doi: 10.1186/1471-2393-10-67
- Fotso JC, Ezeh A, Oronje R. Provision and use of maternal health services among urban poor women in Kenya: what do we know and what can we do? J Urban Health. 2008; 85(3): 428-442. doi: 10.1007/s11524-008-9263-1
- Singh PK, Rai RK, Alagarajan M, Singh L. Determinants of maternity care services utilization among married adolescents in rural India. PLoS One. 2012; 7(2): e31666. doi: 10.1371/journal.pone.0031666
- UNFPA. Achieving the millennium development goals. Population and reproductive health as critical determinants-Population and Development Strategies Series. 2003; 10.
- Merkatz IR, Tharpson JE. The history of prenatal care. In: New prospective on Prenatal Care. Elsevier, NY; 1990.
- Munim S, Rahbar MH, Rizvi M, Mushtaq N. The effect of grandmultiparity on pregnancy related complications: the Aga Khan University experience. J Pak Med Assoc. 2000; 50(2): 54-58.
- Nassar N, Sullivan EA. Australiaʼs mothers and babies 1999. Sydney: AIHW National Perinatal Statistics Unit; 2001.
- Oakley A. The captured womb: A history of the medical care of pregnant women. B. Blackwell; 1986.
- Sarkar P. Unintended Pregnancies in Bangladesh: Levels and Correlates. Journal of Modern Mathematics and Statistics. 2009; 3(4): 78-81.
- Titaley CR, Dibley MJ, Roberts CL. Factors associated with underutilization of antenatal care services in Indonesia: results of Indonesia Demographic and Health Survey 2002/2003 and 2007. BMC Public Health. 2010; 10: 485. doi: 10.1186/1471-2458-10-485
- Richard LB. Peripheral utilization of Glucose in Pregnancy. Obstetrics & Gynecology. 1956; 7(6): 658-664.
- Pembe AB, Carlstedt A, Urassa DP, Lindmark G, Nyström L, Darj E. Quality of antenatal care in rural Tanzania: counseling on pregnancy danger signs. BMC Pregnancy Childbirth. 2010; 10: 35. doi: 10.1186/1471-2393-10-35
- Bassani DG, Surkan PJ, Olinto MT. Inadequate use of prenatal services among Brazilian women: the role of maternal characteristics. Int Perspect Sex Reprod Health. 2009; 35(1): 15-20. doi: 10.1363/ifpp.35.015.09
- Kim HG, Mandell M, Crandall C, Kuskowski MA, Dieperink B, Buchberger RL. Antenatal psychiatric illness and adequacy of prenatal care in an ethnically diverse inner-city obstetric population. Arch Womens Ment Health. 2006; 9(2): 103-107. doi: 10.1007/s00737-005-0117-5
- Diyab EM, Al-Wehibi KM, AL-Nasseri JS, et al. Assessment of Blood Groupʼs Awareness among the Omani Population. Madridge J Nurs. 2018; 3(1): 101-106.