Mini-Review Article
Patient Conducting Model for Nursing Care
Professor, Faculty of Health Sciences and Social Studies, University of Szeged, Hungary
*Corresponding author: Kornélia Helembai, Professor, Faculty of Health Sciences and Social Studies, University of Szeged, Hungary, E-mail: helembai008@gmail.com
Received: January 24, 2019 Accepted: February 21, 2019 Published: February 28, 2019
Citation: Helembai K. Patient Conducting Model for Nursing Care. Madridge J Nurs. 2019; 4(1): 139-144. doi: 10.18689/mjn-1000125
Copyright: © 2019 The Author(s). This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Aim: The aim of this study is to introduce and offer aspects in the field of nursing education with special regard to safety in patient care, where the patent and the nurse work together for success, by highlighting the inherent features of patient conducting required from professional nursing.
Method and Sample: In order to explore the roots and main characteristics of patient conducting, the method of concept analysis was used, based on the qualitative literature review of the most known and accepted theories in the field of nursing and other (counseling, social work) professions requiring a therapeutic relationship.
Results: The findings of the study show definite and mutual equivalences among the values, principles and elements of the assessed helping profession. The evaluation of the core components of the helping professions evidences the importance of the patient conducting process, which creates conditions whereby all patients may preserve their human dignity and identity. Patient conducting ensures patientʼs right to self-determination and all other rights.
Conclusion: Nursing care has to be based on the assumption that the patients are in the best position to resolve their own problems. In this sense, next to excellent technical skills, nurses have to be familiarized with the methods of patient conducting at a high level to fulfil the requirements of professional competence.
Recommendation: Nursing education needs to continually develop and introduce new goals, content, and teaching methods to meet the health care needs of people they serve, with special regard to patient conducting.
Keywords: Helping profession; Nursing model; Patient conducting; Paramedical counseling.
Introduction
The International Council of Nursesʼ 1950 resolution, which is still valid today, states that in countries where nursing is not developed the health status of the population does not reflect the level of development of medicine [1].
The public opinion of the nurses of the world, based on their practical experience grounded in theoretical knowledge, has long defined the essence of nursing by recognizing that the concept of nursing is not simply a list of activities (skill-mixes). Nursing care in all types of healthcare settings working with patients of all age groups has also an intellectual aspect which cannot be delegated [2,3].
Recent studies introduce several indicating factors that urge the need for the involvement of patients in their caring process, since several people from all ages and backgrounds, IQ, income and education levels are not able to understand their own medical information [4]. The lack of recognition and interpretation of patientʼs presenting symptoms were also identified as dangerous influencing factors in getting appropriate treatment for the patient in time [5]. Researchers from the field of the reproductive health highlight different responses between men and woman to the problem of infertility and urge a special attention to patientʼs conducting as supportive therapy by health professionals during the treatment period [6]. Nursing is a helping profession focusing on the human being. The health care service declares patientʼs right to have their dignity respected–including the right to make decisions about accepting help and treatments.
People in need require some conduct with the help of which they can manage and overcome their own difficulties related to their health status. In this respect the collaborative caring process in nursing can be interpreted as a conductive relationship during which the nurse produces an atmosphere conducive to the nursing process. Patients will be able to effectively utilize their internal power to get the best possible health status and quality of life for themselves. For this reason, next to developing outstanding technical skills nurses have to be familiarized with the knowledge of patient conducting structure and counseling at a high quality level to achieve professional competence.
The aim of this study is to offer some grounds for consideration with special regard to the field of nursing and safety patient care, where the patient and the nurse work together by highlighting the inherent features of patient conducting required from the professional nursing.
Need for Patient conducting in Nursing Theories
Highly-qualified nursing professionals in developed health care work closely with patients or patient groups to individualize care and built relationships of mutual regard and trust: instead of “for,” the nurses work together “with” the patients [3]. The qualities of such a helping relationship are: mutuality; reality; feeling; knowledge; concern for the other person; purpose; immediacy; offering something new; and no judgment [7]. In nursing, the central value is human dignity, and each person is respected as a unique individual and supported by the nursing care. Thus in the frame of the offered helping relationship nursing has to be based on the assumption that patients are in the best position to resolve their own problems. The need for patient conducting is not a new idea. In fact, it can be followed over the whole development process of theories of nursing from their beginnings. Furthermore, analyzing several classical and new theories, it can be said that most of them contain one of the five criteria of the client-centered therapy and counseling to create an accepting atmosphere for communicating the respect for dignity and uniqueness of the individual.
Characteristics and criteria of client-centered therapy and counseling in nursing theories
Peplauʼs concept clearly accents the main characteristics of client-centered therapy and counseling and expresses the essential view that nursing is an interpersonal process, and both the patient and nurse have an equally important part in the therapeutic interaction. The nurse must encourage the patient to recognize and explore feelings, thoughts, emotions, and behaviours by providing a non-judgmental atmosphere and therapeutic emotional climate [8].
1st criterion of the client-centered approach: Nurses should build sensitivity and awareness towards client dignity during the whole organization and care giving process. People build their self-image from messages they receive from other people about themselves. People who see themselves as valuable and have a sense of their own strength tend to be more satisfied and have the power to deal effectively and with their environment [9].
Hall highlights the patientʼs needs, feelings and motivation, which inspire the whole nursing process. The nurse seeks to increase patient motivation and awareness to support decision-making based on the patientʼs new level of awareness. Once the motivations are defined, then the patient is the best person to set goals and arrange priorities [8].
2nd criterion of the client-centered approach: Nurses should avoid stereotyping clients. Incoming clients are classified, which reflects the need to generalize and to organize phenomena on the basis of common characteristics during the process of knowledge building. In this case the person becomes and is processed as a category [10].
According to Abdellahʼs interpretation, the clientʼs needs can be viewed as problems, and the quality of nursing care requires that nurses be able to identify and solve overt and covert nursing problems. The client-centered approach calls for the correct identification of nursing problems, which influences the nurseʼs judgment in selecting the next step in solving the clientʼs nursing problem. Thus, routines of care must be reduced to an absolute minimum, allowing room for the patientʼs individuality [8].
3rd criteria of the client-centered approach: All clients have unique wants and needs. Focusing on clientsʼ wants is more useful than focusing on clientsʼ needs. The concept of want is defined by the patients themselves according to their personal values and preferences. Need is defined by the nurse instead of the patient. This distinction is particularly important because the most motivating personal factor for patients is being able to communicate their wants and wishes [11].
Henderson stresses that all people have common needs, but no two patients are exactly alike, so each nurse must interpret human needs as these have meaning to the individual patient. The nurse must identify the need and supply measures that are applicable to that individual [8].
4th criterion of the client-centered approach: Nurses should expect client participation in problem solving. Participation in decision-making, planning, and action on oneʼs own behalf is essential to the maintenance of human dignity. The “rescue-fantasy” in the therapist restricts the patientʼs right to autonomy [12].
Orem emphasizes self-care as a positive action that has both a practical and a therapeutic effect. Self-care may be therapeutic in how it contributes to making adjustments towards achieving universal self-care requirements, to the establishment of new techniques of self-care, and to modifying self-image and the routine of daily life [8].
5th criterion of the client-centered approach: Nurses should assist clients in discovering and making use of their strength. Most clients strive to present themselves as pro-active autonomous human beings who have the ability to enhance their functioning and competence through the use of the helping relationship. Patientʼs reactions are different when the focus is on the personʼs strengths rather than weaknesses [13].
Parseʼs human becoming theory emphasizes how individuals choose and bear responsibility for patterns of personal health, where the patient, not the nurse, has the definitive role and is the decision maker [3].
Integrating the five main characteristics of client-centered therapy above into the conceptual frame of nursing theories, a logical coherence can clearly be seen among them:
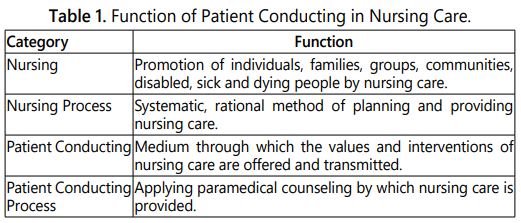
Paramedical counseling in nursing care helps people who are currently having difficulty moving past a point, taking into account the multicultural factors of an environment. It engages a conscious plane and is preventive and supportive in nature. It focuses on the present and it is directed to solving problems in the given nursing situation. The nurseʼs therapeutic role extends to giving advice and information to individuals or groups, helping them in orientation, providing information via therapeutic discussion, helping them in decision-making and assisting individuals and groups in focusing and in using their own potentials and strengths, improved by supportive strategies (Table 1).
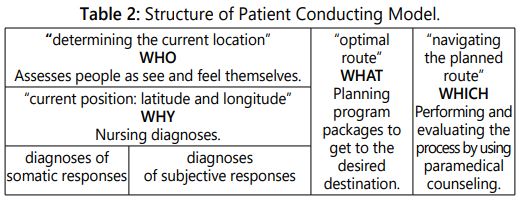
Structure of Patient Conducting Model in Nursing Care (Table 2)
Imagining nursing care through the metaphor of marine navigation, the most vital function is to determine the current location and the optimal route to the destination, and to steer the craft on the planned route. Using the method of triangulation and the coordinates of the current position (latitude and longitude) as well as the target, one can plan the desired route and correct for deviations.
The nurse-patient partnership has a key role in nursing care. It provides a frame for the nurse-patient the interaction which enables mediation and processing of information. The physical status and parameters of the patient, such as blood pressure, BMI, and so on can be measured and registered. Based on these parameters the nursing diagnosis and the necessary modes of intervention can be formulated; furthermore, their implementation can be controlled, and the consequences of mistakes can mostly be revealed as facts. Yet, these indicators “have no face;” only the patientʼs subjective way of responding can tell how they think, feel, and act on the problems. Consequently, there is a significant difference between physical and subjective responses: it is not possible to make a “medical report” on inadequate patient conducting and its consequences. That is why the responsibility of the professionals to validly assess the personal responses of patients, which can be achieved through triangulation, is also a core element of the patient-centered nursing care performed by paramedical counseling [14].
In line with the objective of the study, we now focus on the patient subjective responses, which receives less attention, although are given equal weight with their physical status in measuring the effectiveness of the nursing process.
Patient assessment through patient conducting (WHO)
Creating patient conducting diagnoses follows the logic of somatic diagnosis, the formulation of which requires a novel vision and a high degree of integration of complex knowledge mediated to nurses by education. Patients report verbal and/or non-verbal complaints about their subjectively-experienced status, which they tell their assistants in the form of coded messages. That is why, similarly to physical assessment, it is suggested first to have a general inspection to assess what losses patients have experienced. The types of losses from an objective view are: a) external objects and resources, b) habituated environment, c) important persons, d) immanent elements of the self systemʼs existence, e) own or significant peopleʼs lives [15]. When calculating losses patients use their own perspective to formulate their own needs, which are usually limited to eliminating subjectively-experienced complaints. The numbers of needs assessed through the nurseʼs perspective can far exceed these, as their scope of their perception is much wider owing to their professional knowledge. In addition to the problems reported by the patients, it is therefore necessary to consider the factors that the patients cannot, due to their lack of knowledge and/or excessive proximity to problems.
Diagnosing patient responses by decoding the sent messages (WHY)
An important element of patient conducting and diagnosis is the understanding and decoding the messages and complaints of adult and mentally not disturbed patients, which call for the identification of subjective responses. The patientʼs basic attitudes toward their sickness and/or nursing situation can be decoded through their messages, and some special types and characteristics of these can be defined [16] (Figure 1).
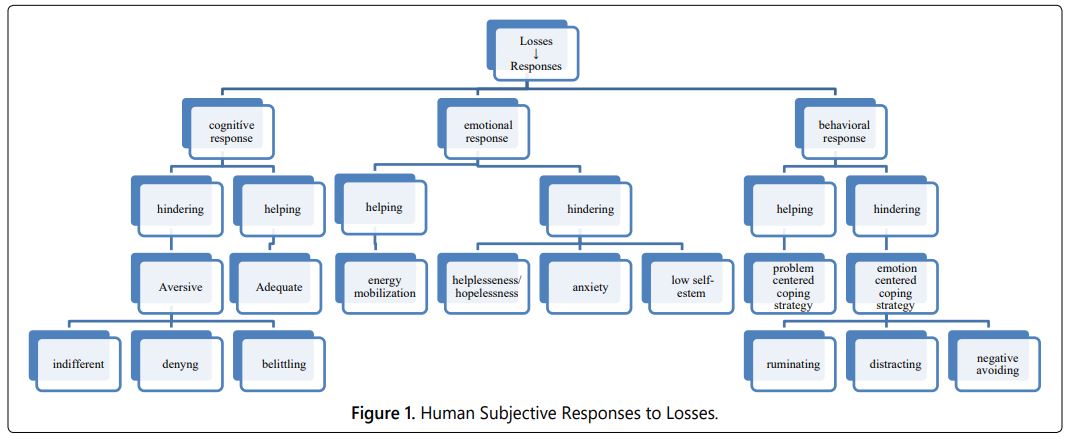
In the cognitive dimension the following attitude forms can be identified:
Adequate: the patients accept the rules and an obligation related to their health problems to use their power to further their recovery.
Aversive: the patients are not ready or are not able to face their sickness, which can appear as: a) the patients show an indifferent attitude toward their health status, b) the patients have a tendency to belittle the implication of their health problem or c) the patients flatly deny the existence of their health problem.
The main emotional statuses such as anxiety, helplessness/hopelessness and low self-esteem also appear during the interaction, so they are also worth observing and identifying, as they can be used to define the characteristics relatively well [17].
Coping strategies also need particular attention in order to assess patient conducting. Patients facing a health problem are under stress. The factors that influence the interaction between people and stressors are predictability and the ability to control the internal and external events and initiate the coping mechanisms. a) A problem-centered strategy helps people focus on the problem-solution, take into account the helping factors, and initiate changes in their internal and external environment. b) Emotion-focused strategies put the focus on the patientʼs feeling rather than on problem-solving. These include ruminating, distracting and negative avoiding coping strategies [16].
Aspects of planning nursing conducting (WHAT)
Look at your palm: the lines are well visible on it. Now take your palm and slowly put it to your nose – the lines become blurry, because they are too close for you to see them clearly.
One of the quality indicators of the design phase is the common ‘problem list’ created as a result of joint work between patient and nurse, which contains the wants of the patient and the needs assessed by the nurse in a coordinated manner. Patients should always be able to clearly see and know their reasons and opportunities, on the basis of which “program packages” can be designed with their active participation. It is advisable that programs outlined with patientʼs participation-in accordance with the medical interventions, taking into account the current needs together with the previous personal life experiences of the patients-should be prepared according to the priorities of the health needs on a daily basis. This, on the one hand, helps therapists to systematically monitor the patientʼs development, and, on the other hand, this knowledge gives patients a sense of predictability and being able to influence their own care.
The needs assessed by nurses should be accepted by patients as their own demands; therefore, reconciling the needs and the demands assessed can be considered a milestone in the cooperation, as this helps patients to understand their situation and the aims and significance of the nursing diagnosis and interventions [8].
For each item of the common need/demand list developed, it is necessary to disclose how patients are currently dealing with a particular sub-problem or the proposed interventions and program packages.
Characteristics of patientʼs subjective responses may be significantly different for each program point, even day to day or hour to hour. Therefore, in the course of patient conducting, in connection with each task assigned to the different problems and diagnoses, nurses have to clarify the attitude of the patients/relatives to the situation, their emotional statuses that might influence their decisions, as well as their coping strategies.
With the help of specific programs designed for each day, patients can participate consciously in their own healing process, not feeling that they are merely obeying the regulations of the care providers [18].
Implementing paramedical counseling in nursing care: (WHICH)
To tell - it does not mean to hear! To hear - it does not mean to pay attention! To pay attention – it does not mean to understand! To understand – it does not mean to agree! And to agree – it does not at all mean to make it happen!! [19-21].
With the help of the program packages based on diagnoses program packages that can contribute to the improvement of the patientʼs condition are planned. Interventions and recommendations can be clearly formulated. Local pressure can result a temporarily ‘obedient’ patient behaviour but they do not feel the decision to be their own.
The strategies used to conduct patients can help nurses to enable patientʼs commitment to healing. In the absence of this, persuasion becomes only ‘nagging’ and encouragement becomes ‘hushing’. In this form, despite an enormous energy investment, the result is usually extremely modest, as patients will adhere to the instructions a passively and all players will feel frustrated and inadequate. Therefore, it is necessary to implement appropriate counseling strategies to enable patients and their relatives to have a clear understanding of their current situation, which without assistance is often too close to be able to gauge realistically the assisting and inhibiting factors and the available opportunities.
In a classical interpretation, the helping relationship is the tool of helping professions, in which the individual moves to solve the problem with the help of a professional counselor. Professional helpers, having a qualification in higher level counseling training and direct experience in a field, contribute to solving human problems in different situations. Nursing care is a series of interactions designed to help solve specific problems related to the nursing situation. This requires the flow of information, which is mainly realized through paramedical counseling using the different facilitating and supportive strategies [22].
One of the basic guarantees of safe patient care is the involvement of patients and their active participation in the healing process. Paramedical counseling helps people to integrate the content they want to convey into the affected peopleʼs own approach and experience system. As a result, they will have the opportunity to consciously reflect on and manage their own situation and future opportunities; otherwise, they are simply left out of their own healing history. This is why recognizing the significance of nurseʼs role in counseling is essential in order that nurses not to work for their patients or clients but to work together with them to achieve common goals [3].
Evaluating the effectiveness of patient conducting
Imagine offering a cooking course to help someone develop their cooking skills using the raw materials they bring. Depending on the raw materials, we take into account the possible menus together and choose the one we want to prepare. We have to decide on the necessary ingredients, tools and spices. A detailed overview and discussion of the steps of preparing the jointly-selected menu establishes the individual tasks of each person involved. After we come to an agreement, we work together in such a way that the food we prepare is close to the taste of the individual, because after all the food has to be prepared and eaten by the person who asked for our help.
The effectiveness of patient conducting can be tracked in the development of patient/client (significant person of patient) knowledge and skills, and in the changes in offered programs and coping strategies deal with losses. People, if they feel that they trust their abilities, can utilize their efforts better. Effective practical application of theoretical knowledge and skills of counseling work will make a significant contribution to the awareness of the importance of a helping relationship, which is also important for the patient/client. Therefore, the mutual summaries of the patientʼs experience of the programs and nurseʼs congruent reflections on the patientʼs development are very important phases in raising the awareness of the patientʼs own efforts and recognizing the meaning of the offered relationship. A credible summary by therapists of the joint work done greatly helps individuals to preserve their human dignity and identity, and to regain and/or retain their independence. The patientʼs development lists also show the results of therapistsʼ work and contribute to the improvement of their experience in counseling. As no two people are identical, so no two cases are identical. The work of nurse therapists is not algorithmic, and this characteristic feature shapes the beauty and difficulty of the profession and also its high degree of freedom and responsibility.
Conclusion
Nurses, doctors and other therapists have to establish a permissive relationship in which the patients/clients feel free to discuss their problems and to obtain insight into them. In this approach the collaborative caring process in nursing can be interpreted as a conductive relationship during which the nurse helps produce an atmosphere that contributes to the nursing process. With the help of this process, patients will be able to manage their internal power to achieve the best possible health status and quality of life for themselves. In this sense, beside excellent technical skills, nurses have to be familiarized with patient conducting at a high level to fulfil the requirements of professional competence.
Recommendation
Nursing education needs an urgent revision. Delaying this would delay innovations in nursing culture anticipated for the 3rd millennium. Secondly, delaying innovation hinders the cost effectiveness of health care services, because without it patients are not ready to use the health care services effectively, leading them to return for further treatment when they are more sick and hopeless. Thirdly, it must not be forgotten that in countries where nursing is not developed, the health condition of the inhabitants does not reflect the level of the development of medicine [1].
Conflict of Interest Statement
The author declared that the submitted article under title Patient Conducting Model for Nursing Care, that there is no conflict of interest, it is my own original till not published work.
References
- Henderson V. Basic principles of nursing care. Basel: S. Karger for International Council of Nurses; 1969.
- Kozier B, Erb G, Berman A, et al. Fundamentals of Nursing. Concept, process and practice. Harlow, UK: Pearson Education Ltd; 2012.
- Georgia Health News. Health Literacy: Many patients donʼt understand what their doctors mean. Accessed March 20, 2013.
- Mellor RM, Bailey S, Sheppard J, et al. Decisions and delays within stroke patientʼs route to the hospital: a qualitative study. Ann Emerg Med. 2015; 65(3): 279-287.e3. doi: 10.1016/j.annemergmed.2014.10.018
- Szatmári A, Fejes Z, Király I. [Menʼs knowledge of male infertility and the possibilities for supporting therapy: risk factors and individual responses]. Orv Hetil. 2018; 159(31): 1262-1268. doi: 10.1556/650.2018.31132
- Keith-Lucas A. Giving and taking help. North American Association of Christians in Social Work; 1994.
- George JB. Nursing theories the base for professional nursing practice; the Nursing Theories Conference Group. Englewood Cliffs Prentice-Hall Inc; 1985.
- Rose AM. Human behavior and social process: An Interactionist Approach. Houghton Mifflin; 1962.
- Toch H. The Care and Feeding of Typologies and Labels. Federal Probation. 1970; 34: 15-19.
- Dumont M. The absurd healer: perspectives of a community psychiatrist. New York, NY: Viking Press; 1971.
- Maluccio AN. Learning from Clients: Interpersonal helping as viewed by client and social workers. New York, NY: Free Press; 1979.
- Potter PA, Perry AG. Basic Nursing: Theory and Practice. Mosby-Year Book Inc; 1991.
- Carpenito LJ. Nursing Diagnosis- Application to Clinical Practice. 14th edition. Philadelphia, PA: Lippincott Williams & Wilkins; 2013.
- Anderson, RM, Funnell MM. Patient empowerment: myths and misconceptions. Patient Educ Couns. 2010; 79(3): 277-282. doi: 10.1016/j.pec.2009.07.025
- Battay M, Toth P. Winning words and convincing? A strategy for authentic communication. Business & Cafe. 2016.
- Braddock R. An Extension of the “Lasswell Formula”. J Commun. 2006; 8(2): 88-93. doi: 10.1111/j.1460-2466.1958.tb01138.x
- Lasswell HD. The Structure and Function of Communication in Society. 2006; 1: 84-95.
- Hackney H, Cormier LS. Counseling Strategies and Interventions. 3rd edition. Prentice Hall, 1987.